Abstract
Introduction:
Disseminated Intravascular Coagulation (DIC) is a systemic pathophysiologic process which occurs in response to an underlying inciting event resulting in a complex interaction between the inflammatory and coagulation pathways. The development of DIC inpatient is often an ominous prognostic indicator with fulminant cases resulting in bleeding and widespread thrombosis ultimately resulting in death. It is not a disease by itself, but rather a sign of underlying disease incited by causes such as sepsis, acute pancreatitis, leukemia, burns, crush injuries, solid tumors, and viral illnesses. The purpose of this study is to identify the annual trends in mortality and morbidity associated with DIC in hospital and its association with specific etiologies.
Methods:
Using the National Inpatient Sample (NIS) for years 2002-2014, DIC was defined as ICD-9 code 286.6 for a primary or secondary diagnosis in conjunction with ICD-9 and clinical classification software codes to identify the most common etiologies of DIC. Linear regression analysis was used to assess the annual trends in incidence and mortality. We employed univariate logistic regression analysis to calculate odds ratios (OR) for the most common causes of DIC and their relationship with mortality.
Results:
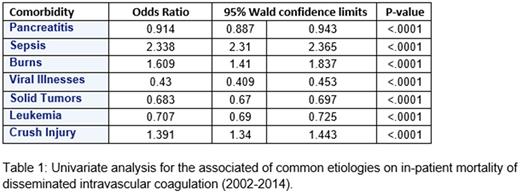
Among in-hospital admissions between 2002 and 2014, 101,030 patients (N=481,657, weighted) developed DIC. Annual incidence has been increasing steadily from 28,119 in 2002 to 43,570 in 2014. Mortality has remained relatively unchanged at 47% in 2002 and 45% in 2014 (p <0.0001). The mean length of stay (LOS) remained unchanged from 14.10 to 14.25 (p = 0.6369), however the total costs of admission increased from $94,726 to $226,929. Sepsis was associated with 55.5% of all incdiecnes of DIC, pancreatitis 3.7%, burns 0.19%, viral illnesses 1.7%, solid tumors 10%, leukemia 5.8%, and crush injuries 2.4%. A univariate analysis identified an increase association between mortality and etiologies such as sepsis (OR=2.34), burns (OR=1.61), and crush injuries (OR=1.39). A decreased mortality was seen with viral (OR=0.44), leukemia (OR=0.71), solid tumors(OR=0.68), and pancreatitis (OR=0.91).
Conclusion:
Our study indicated that among the patients admitted with DIC between 2002 and 2014, there was a significant increase in annual incidence while mortality and length of stay remained the same. Notably, the total costs of admissions associated with DIC more than doubled. Sepsis is by far the most commonly associated comorbidity in these patients, and also associated with a higher mortality. Burns and crush injuries also had higher mortalities, while the lowest mortality was seen in viral illnesses and cancers. Due to the highly variable course and high mortality associated with DIC extra vigilance should be exercised when identifying the cause of DIC and the expected course.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal